Midwifery is a profession that belongs to the medical sciences and deals with pregnancyand childbirth, including the care of the newborn, in addition to the sexual and reproductive health of women throughout their lives. A practitioner of obstetrics is known as a midwife. The uniform worn by the (male) midwife consists of blouse and trousers and is usually pink and pale blue in color.
A 2013 meta-analysis by the Cochrane Foundation concluded that most women should be offered obstetrical standards of care and be encouraged to seek this option, although due care should be taken in applying this counseling to women with significant medical or obstetrical
The analysis indicated that obstetric care was associated with a reduction in the use of epidural serum, fewer episiotomies or instrumental deliveries, and a reduced chance of fetal loss before 24 weeks’ gestation. However, this type of care has been associated with an increase in the average length of labor measured in hours.
Scope of Obstetrics
Gestation
- First Trimester
The first trimester exams vary from country to country. A Pap test and a general urine test, blood tests including a general blood test, blood grouping (including a rhesus test), tests for syphilis, hepatitis, HIV and rubella are performed. In addition, tests for chlamydia can be done with a urine sample, and tests for sickle cell anemia and Mediterranean anemia in women who belong to high-risk groups. Women’s consent is needed before the necessary tests. Blood pressure, height and weight are also measured. Previous pregnancies as well as family, social and medical history are discussed. Women can also have an ultrasound scan during the first trimester to calculate their estimated due date. Some can do genetic testing, such as tests for Down syndrome. Issues such as diet, exercise and discomforts such as morning sickness are also discussed.
- Second Trimester
The pregnant woman visits the (male) midwife monthly or more often during the second trimester. The partner of the expectant mother may accompany her. The (male) midwife will discuss pregnancy issues such as fatigue, heartburn, varicose veins and other common problems such as back pain. Blood pressure and weight are monitored, and the (male) midwife measures the pregnant woman’s abdomen to see if the fetus is developing as expected. Laboratory tests such as general urine test, general blood test and glucose tolerance test are done in the event that the (male) midwife deems it necessary.
- Third Trimester
In the third trimester the (male) midwife will see the pregnant woman every two weeks until the 36th week and on a weekly basis after that time. Weight and blood pressure will be checked, and abdominal measurements will be taken. Laboratory tests such as a general blood count and a general urinalysis may be done along with additional tests for high-risk pregnancies. The (male) midwife palpates the woman’s abdomen to determine the position of the fetus. A pelvic exam may be done to show if the cervix is dilating. The (male) midwife and prospective mother discuss birthing options and develop a birth care plan.
Childbirth
Labor pains and childbirth
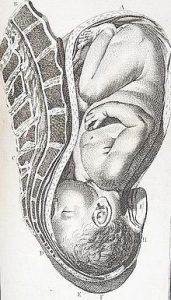
A demonstration of the normal position of the fetus before delivery. The membranes have ruptured and the cervix is fully dilated.

Newborn rests while midwife checks breathing.
Midwives are qualified to assist in a normal vaginal delivery while more complex cases are handled by medical staff with more specialized training. Labor is divided into four stages:
- First stage of labor: During the first stage of labor the pregnant woman begins to feel strong and regular contractions which come every 5-20 minutes and last 30 to 60 seconds. Contractions gradually become stronger, more frequent and last longer until the cervix is fully dilated to 10 cm.
- Second stage of labor: During the second stage the infant begins to descend from the birth canal. As the infant moves toward the entrance of the vagina, its head can be seen. In the past, an episiotomy (an incision in the tissue at the entrance of the vagina) was done as part of the procedure as it was believed to prevent excessive dilation and to heal more completely than a natural dilation. However, more recent research suggests that a surgical incision may be more extensive than a natural tear and is more likely to contribute to later incontinence and pain during intercourse than a natural tear would.
The (male) midwife assists the baby and when it has fully emerged, she cuts the umbilical cord. If requested, the father can cut the cord. In the past, the cord was cut almost immediately after birth, however there is increasing evidence that delayed cutting may benefit the infant.
- Third stage of labor: During the third stage, the placenta emerges from the uterus.
- Fourth stage of labor: The fourth stage of labor is the period that begins immediately after delivery and lasts for about 6 weeks. The World Health Organization describes this period as the most critical but also the most neglected phase of a mother’s and infant’s life. For years, infants were typically removed from their mothers after birth, but since 2000, some authorities have begun to recommend that early infant-mother physical contact (placing the naked infant on the mother’s breast) benefits both. Since 2014, physical contact has been endorsed by all institutions responsible for the welfare of infants. Thus, to aid bonding as well as successful breastfeeding, the (male) midwife observes directly as the infant lies on the mother’s breast and removes it for further observations only after its first feed.
After the birth, if the mother had an episiotomy or has a tear in the perineum, this is sewn up. The (male) midwife regularly monitors the contraction of the uterus, its size and vaginal bleeding. Throughout labor, the mother’s vital signs (temperature, blood pressure and heart rate) are closely monitored and fluid intake and output are measured. The (male) midwife also monitors the baby’s heart rate, palpates the mother’s abdomen to monitor the position of the fetus and performs vaginal checks when necessary. If labor deviates from normal at any stage, the (male) midwife seeks help from more qualified staff.
Childbirth Positions
Until the previous century, a variety of positions were used for childbirth. The lithotomy position was only used after the advent of forceps in the 17th century, and since then childbirth has been transformed from a supportive experience at home to a medical intervention in the hospital. There are significant advantages to adopting a vertical birthing position, such as stronger and more efficient contractions, which aid cervical dilation, increased pelvic diameter, and improved uterine contractility. Upright positions in the second stage include sitting, squatting, kneeling, and being on hands and knees. Stage two upright posture includes sitting in a chair, squatting, kneeling, and standing on hands and knees.
Postnatal Period
For women who have given birth in a maternity hospital, the minimum stay for observation in it is 6 hours. Those who leave early do so against all medical advice. They can also choose when to leave the maternity ward. Complete postpartum assessments are performed daily in hospitalized women, or more frequently if needed. A postpartum assessment includes external observation of the woman, general physical condition, breastfeeding (either discussion and assistance with breastfeeding or discussion of suppression of lactation), palpation of the abdomen (in case of normal vaginal delivery) to check for uterine prolapse, or check for cesarean section (clothing does not need to be removed), check of the perineum (especially if lacerations or sutures are present), review of her cesarean, confirmation that both the urinary and digestive systems are functioning and look for symptoms of thrombosis in the central internal arteries. The infant is also checked for jaundice, signs of adequate breastfeeding, or other worrisome conditions. The infant undergoes a newborn exam between 6 and 72 hours after birth to check for conditions such as heart failure, defective hips, or eye problems.
Within the community, the (male) midwife visits the woman until the tenth day. This does not mean that she sees the woman and the infant daily, but that she cannot release them from her care until the tenth day at the earliest. Postnatal checks include newborn tests around the fifth day. The baby is weighed and the (male) midwife plans visits based on the health and needs of the mother and baby. Then they come under the supervision of the visiting doctor.
Newborn Care
At birth, the infant receives an Apgar score at an age of, at least, between one and five minutes. This is a 10-point scale that assesses the infant in 5 different areas—each with a value between 0 and 2 points. These areas are: color, breathing difficulty, complexion, heart rate and response to stimuli. The (male) midwife checks the baby for any obvious problems, weighs the baby and measures the head circumference. The (male) midwife makes sure the umbilical cord is securely tied and the baby has the appropriate tags on it (if in hospital). You do not measure the length of the infant on a regular basis. The (male) midwife performs these checks as close to the mother as possible and returns the infant to the mother. Physical contact is encouraged as it regulates the infant’s heart rate, breathing, oxygenation and temperature and promotes infant-mother bonding and breastfeeding.
Midwifery Care Coordination
Midwifery care coordination is the process where one or more midwives have primary responsibility for the coordination of care for pregnant women with a multidisciplinary network of consultation and referral to other health professionals. This is different from ΄΄medical care΄΄ where an obstetrician or family doctor is primarily responsible. In participatory models of care, responsibility is shared between the midwife, obstetrician and/or family doctor.
According to a Cochrane meta-analysis of public health systems in Australia, Canada, New Zealand, Ireland and the United Kingdom, “most women should be offered obstetrical standards of care and women should be encouraged to seek this option, although due care should be taken in applying this advice to women with significant medical or obstetric complications”.
Among the results of obstetric care are the following:
- a reduction in the use of epidural serum, with fewer episiotomies or instrument-assisted deliveries.
- longer average duration of labor, measured in hours.
- increased chances of care during childbirth by a (male) midwife familiar to the pregnant woman.
- increased chances of spontaneous vaginal delivery.
- reduced risk of premature birth.
- reduced risk of miscarriage before 24 weeks’ gestation, although there does not appear to be any difference in the same risk after this time.
There was no difference in the number of cesarean sections. All trials in the Cochrane Foundation’s analysis included licensed midwives, and none included traditional midwives. Also, no trials included out-of-maternity deliveries.
Labor market
Employment Sectors and Labor Market Prospects
The (male) midwife may work:
- in private and public maternity wards – Hospitals,
- gynecological clinics,
- assisted reproduction centers,
- private clinics,
- breastfeeding or painless childbirth companies,
- neonatal units & neonatal care,
- Family Planning Department of Hospitals,
- in Surgeries Participating in the Surgical Team e.g. (Genna) etc.,
- health centres.
(Male) Μidwives can also work as freelancers offering their services at the home of the pregnant woman or mother, and the newborn, mainly in villages and semi-urban areas, after they have practiced their activities for two years in a hospital or other health institution accredited for this purpose.
A license is then granted by the Ministry of Health, Welfare and Social Insurance.
The (male) midwife can also practice the profession in all the countries of the European Union according to the respective provisions.
